Our research and literature review of PBC suggest that most of the difficulties for effective GP commissioning are related to structures, mechanisms and professional practices that resist and conflict with collaborative and integrated modes of commissioning and delivering services. PBC has managed to achieve some good results where these barriers were overcome, where there was greater stakeholder engagement, and where the purchasing power of the PBC groups was strong enough to prevail over internal conflicts of interest. Many of the conflicts encountered were between commissioning consortia and the PCTs, but low motivation and engagement of ‘rank and file’ GPs, hospital consultants and key local organisations also contributed to difficulties encountered in the development and implementation of service redesigns.
In many cases the local significance and overall effectiveness of PBC projects and interventions have not yet been fully appreciated or demonstrated. Many interventions are driven by the need to reduce expenditure and seem to be focused mainly on addressing excessive referrals and prescribing. While this is necessary in the difficult economic climate, few systemic interventions are evident which attempt to create new models of care, missing the potential for wider, organisational efficiency gains. In addition patient knowledge is often limited to data analysis or the involvement of disease specific patient groups, while effective engagement of the general public has not been fully developed and integrated into commissioning processes.
The proposals in the Health White Paper for enhanced responsibility for GP commissioning consortia and the quality focus of the new provider remuneration systems (DoH 2010a), is intended to ‘liberate’ GPs from the control and potential blockage of PCTs and reduce conflicting interests with the acute services. It has been recognised, however, that the major organisational changes involved may also create a vacuum of competencies and supporting frameworks that needs to be adequately filled and rebuilt. We consider this transition period as an occasion to re-think GP commissioning from a wider perspective:
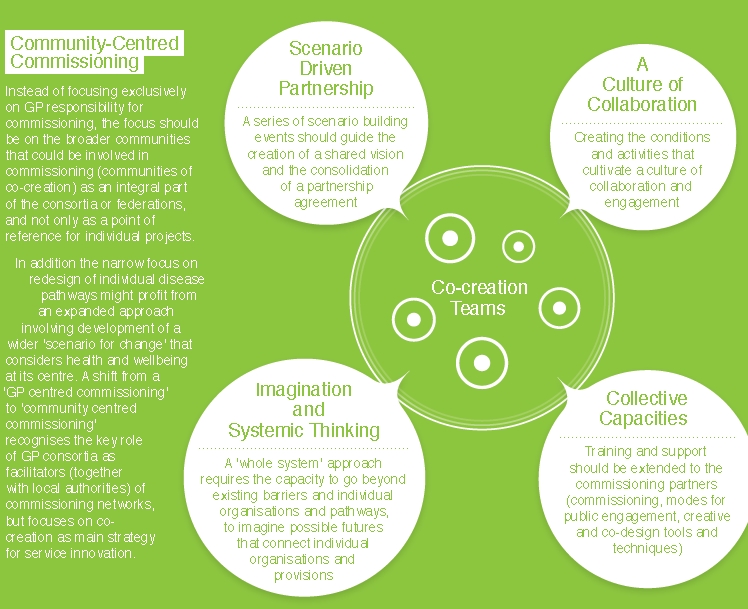
Instead of focusing exclusively on GP responsibility for commissioning, the focus should be on the broader communities that could be involved in commissioning (communities of co-creation) as an integral part of the consortia or federations, and not only as a point of reference for individual projects. In addition the narrow focus on redesign of individual disease pathways might profit from an expanded approach involving development of a wider ‘scenario for change’ that considers health and wellbeing at its centre. A shift from a ‘GP centred commissioning’ to ‘community centred commissioning’ recognises the key role of GP consortia as facilitators (together with local authorities) of commissioning networks, but focuses on co-creation as main strategy for service innovation.